BMI and Risk Factors for Chronic Diseases: Understanding the Link
Body Mass Index (BMI) is a measure that relates an individual’s weight to their height, providing a general indication of body fat and categorizing individuals into different weight status groups. Understanding BMI and its association with chronic diseases is crucial, as higher BMI categories are linked to increased risks of various health conditions. This article explores the relationship between BMI and common chronic diseases, highlighting key risk factors, implications, and preventive strategies.
Understanding BMI:
BMI is calculated by dividing an individual’s weight in kilograms by the square of their height in meters (BMI = weight / height^2). It classifies individuals into the following weight status groups:
- Underweight: BMI less than 18.5
- Normal weight: BMI between 18.5 and 24.9
- Overweight: BMI between 25 and 29.9
- Obese: BMI 30 or higher
While BMI provides a general assessment of body fatness, it does not differentiate between fat mass and muscle mass, nor does it account for factors such as body composition or distribution of body fat.
BMI and Chronic Disease Risks:
- Cardiovascular Diseases:
- Hypertension (High Blood Pressure): Excess weight, particularly abdominal obesity (central obesity), increases the risk of hypertension. High blood pressure strains the heart and blood vessels, leading to cardiovascular diseases such as coronary artery disease and stroke.
- Dyslipidemia: Obesity is associated with abnormal blood lipid levels, including high LDL cholesterol (bad cholesterol) and triglycerides, and low HDL cholesterol (good cholesterol), which contribute to atherosclerosis (hardening and narrowing of arteries).
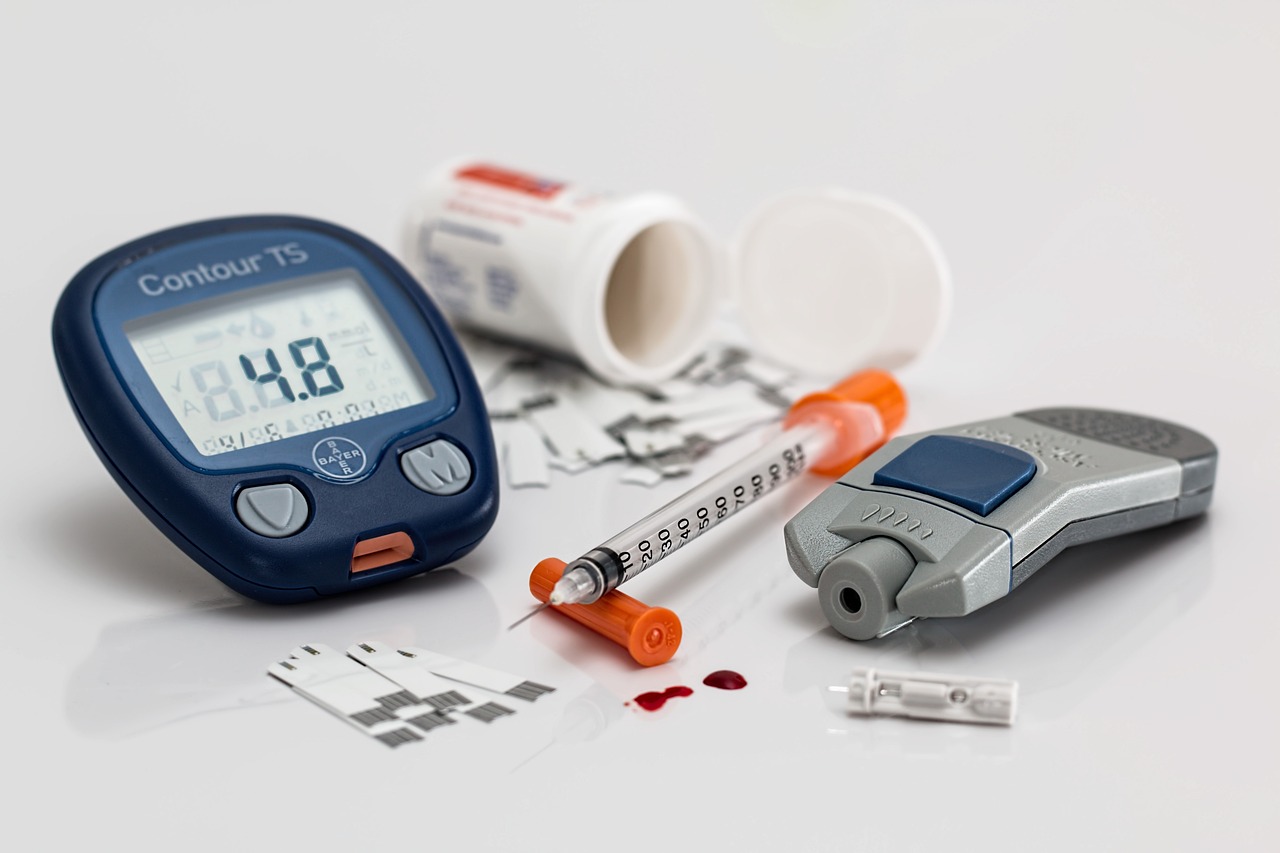
- Type 2 Diabetes:
- Insulin Resistance: Obesity-related insulin resistance impairs the body’s ability to regulate blood sugar levels, leading to elevated blood glucose levels and an increased risk of developing type 2 diabetes.
- Respiratory Disorders:
- Obstructive Sleep Apnea (OSA): Excess weight, especially in the upper body and neck, increases the risk of OSA, a sleep disorder characterized by pauses in breathing during sleep. OSA is associated with hypertension, cardiovascular disease, and daytime fatigue.
- Musculoskeletal Disorders:
- Osteoarthritis: Obesity increases mechanical stress on weight-bearing joints such as the knees and hips, leading to osteoarthritis. Joint pain and reduced mobility are common complications.
- Cancers:
- Breast, Colon, and Endometrial Cancer: Obesity is a risk factor for various cancers, including postmenopausal breast cancer, colorectal cancer, and endometrial cancer. Adipose tissue (fat cells) secretes hormones and inflammatory substances that may promote cancer cell growth.
- Psychological and Social Implications:
- Mental Health Disorders: Obesity is associated with an increased risk of depression, anxiety, and low self-esteem. Psychological factors related to body image and societal stigma may affect mental well-being.
Preventive Strategies:
- Maintain a Healthy Weight:
- BMI Management: Aim for a healthy BMI through balanced nutrition, regular physical activity, and lifestyle modifications to reduce chronic disease risks.
- Healthy Eating Habits:
- Nutrient-Rich Diet: Consume a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting saturated fats, trans fats, added sugars, and sodium.
- Regular Physical Activity:
- Aerobic Exercise: Engage in moderate-intensity aerobic activities (e.g., brisk walking, jogging, swimming) for at least 150 minutes per week to promote cardiovascular health and weight management.
- Strength Training: Incorporate resistance exercises (weightlifting, bodyweight exercises) to build muscle mass, improve metabolism, and support bone health.
- Behavioral Changes:
- Portion Control: Monitor portion sizes and practice mindful eating to manage caloric intake and prevent overeating.
- Stress Management: Practice relaxation techniques such as deep breathing, meditation, or yoga to reduce stress levels and support overall well-being.
- Regular Health Check-ups:
- Health Monitoring: Monitor blood pressure, blood glucose, cholesterol levels, and BMI regularly. Consult healthcare providers for preventive screenings and personalized risk assessments.
Conclusion:
BMI serves as a valuable tool for assessing weight-related health risks and understanding the association between higher BMI categories and chronic diseases. By adopting healthy lifestyle habits, including balanced nutrition, regular physical activity, and preventive health measures, individuals can reduce their BMI, mitigate chronic disease risks, and improve overall quality of life. Understanding the impact of BMI on health empowers individuals to make informed decisions and take proactive steps towards achieving optimal health outcomes. Regular monitoring and consultation with healthcare professionals play a crucial role in managing BMI and promoting long-term health and well-being.